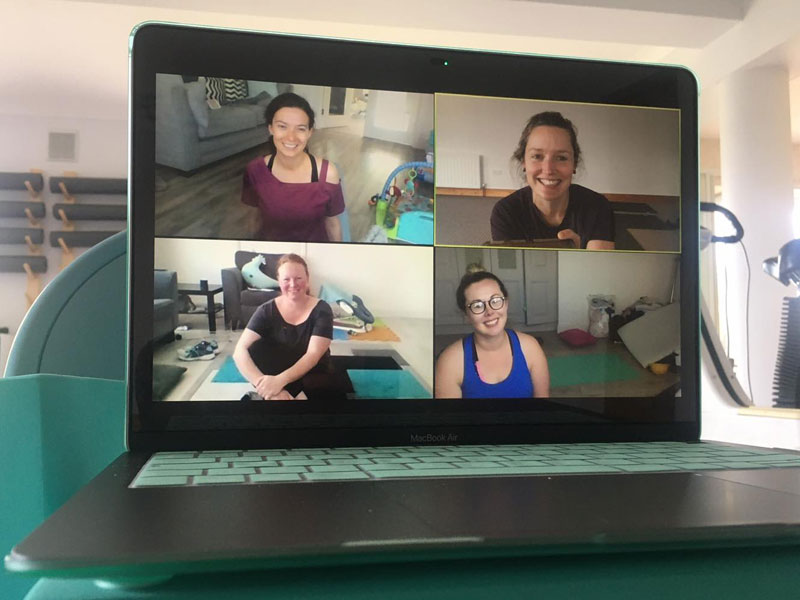
So much change in what is “normal life” over the past few months – Right?! Chatting to or playing games with friends and family using video-chat is becoming common in most households. Like that our health and physiotherapy care too is adjusting.
Although essential face to face health care services are continuing, little of my work truly is essential. Initially when social distancing measures were implemented, I wanted to justify the need for YOUtherapies’ services as being essential for people’s mental and physical health. Which I still argue they are but now I realise the benefits can still be gained while social distancing. Most of a physiotherapy consultation is about listening to you and guiding and supporting you through the changes needed to improve your situation be that through lifestyle changes, exercise prescription or activity modifications.
I’ve researched the merits and flaws of online sessions compared to face to face and included here is a summary of a few systematic reviews and meta analyses (that means they are already summarising all the randomised controlled trials).
Adamse et al (2018) included 16 trials from 2000-2015 that compared exercise based telemedicine to no intervention or to usual care in adults with chronic pain. Meta analyses showed that telemedicine showed significantly lower pain scores and less limitation to people’s activities of daily living versus no intervention at all. There were no differences between telehealth and usual care with regard to pain, physical activity.
With similar favourable results Cottrell et al’s 2017 review included 13 studies (n=1520-many we’re post surgical) and pooled the results. They found that telerehabilitation is effective in improving physical function and equally as effective as face to face sessions. Improvement in the patients’ pain also improved as much with telerehabiliation compared to usual care.
O’Brien et al reviewed 23 studies (n=4994) up until 2018 that looked at phone consultations with supplementary material (info sheets or some had face-face also). Phone consultations improved pain intensity as much as usual care or face to face sessions in people with osteoarthritis and spinal pain. Typical intervention time was between 6weeks-6 months. Phone intervention = education and guidance for self management. Out of five studies that looked at dosage: Three studies found the more calls the better outcome but two studies actually reported that the number of calls did not affect the outcome.
What does all of this mean?
videoPHYSIO is as good as in person management and definitely better than doing nothing at all and even one session might be beneficial
REFERENCES:
Adamse C, Dekker-van Weering MGH, van Etten-Jamaludin FS, Stuiver MM. The effectiveness of exercise-based tel.medicine on pain, physical activity and quality of life in the treatment of chronic pain: a systematic review. Journal of Telemedicine and Telecare. 2018 Sep;24(8):511-526
Cottrell MA, Galea OA, O’Leary SP, Hill AJ, Russell TG. Real-time telerehabilitation for the treatment of musculoskeletal conditions is effective and comparable to standard practice: a systematic review and meta-analysis. Clinical Rehabilitation. 2017 May;31(5):625-638
O’Brien KM, Hodder RK, Wiggers J, Williams A, Campbell E, Wolfenden L, Yoong SL, Tzelepis F, Kamper SJ, Williams CM. Effectiveness of telephone-based interventions for managing osteoarthritis and spinal pain: a systematic review and meta-analysis. PeerJournal. 2018 Oct 30;6:e5846