What is it?
Osteoarthritis (OA) is the most common form of arthritis (Mora et al., 2019), affecting approximately 25% of adults. This prevalence increases with age. It is a degenerative joint disease that causes progressive damage to articular cartilage and surrounding structures of the joint. OA is characterised by breakdown of cartilage, pain and stiffness in the affected joint(s). Articular cartilage is a tough layer of connective tissue that covers the ends of the bones where they articulate with each other within a joint.
OA can affect any joint in the body but mostly affects knees, hips, hands and wrists and neck. Even if you have arthritis in your joints, you will feel your best when keeping active and moving your joints. Remember, movement is medicine!
How does it occur?
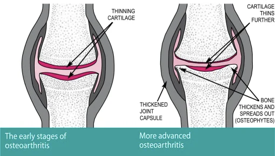
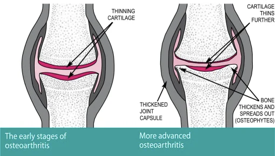
In healthy joints, cartilage covers the end of each bone which provides a nice smooth, gliding surface for the joint to move. In OA, this cartilage breaks down over time which can cause pain, stiffness and swelling of the joint. This process causes inflammation to occur in the body which can feed into the degradation process occurring in the joint.
 It has long been thought that cartilage once worn would not heal but now experts believe that that movement and walking can create more fluid flow around the joints and special cells called chondrocytes help cartilage repair and growth to occur (Moseley, Butler and Stanton, 2023). So instead of calling it ‘wear and tear’ let’s now call it ‘wear and repair’!
It has long been thought that cartilage once worn would not heal but now experts believe that that movement and walking can create more fluid flow around the joints and special cells called chondrocytes help cartilage repair and growth to occur (Moseley, Butler and Stanton, 2023). So instead of calling it ‘wear and tear’ let’s now call it ‘wear and repair’!
The exact cause of OA is not known, however the following risk factors are thought to be linked to the development of OA. It’s important to note that if you have some of these risk factors, it does not mean that you definitely have osteoarthritis.
- Age: people usually develop OA after 40 years of age, although younger people can develop it too.
- Gender: Females are more likely to get OA than males.
- Genetics: Some forms of OA have a strong familial link while others may be more linked to lifestyle factors
- Obesity: Excess weight puts added pressure on the weight-bearing joints. Also, fat tissue produces proteins that can cause inflammation around the joint.
- Joint injury: A major injury or operation may lead to the development of OA later in life
- Joint alignment: The alignment of the joint can possibly cause OA to develop in later years. Some commonly seen alignment issues in the knees can be “knock-kneed” (valgus alignment) or “bow-legged” (varus alignment).
- Weak muscles: If a joint is unsupported by its surrounding muscles, it may be prone to injury and changes in alignment, which can lead to OA.
- Occupation: If your job causes repeated stress on the joint, you may develop OA.
(Mayo clinic 2021; Arthritis Ireland 2021)
It can be useful to recognise the modifiable factors, such as extra weight or weak muscles. These are things you can work on changing and help reduce your chance of developing OA. It may also help improve or control your symptoms of OA if you have already been diagnosed.
How can I recognise OA?
The main signs and symptoms to look out for are:
Stiffness
- Often noticed in the morning or after being inactive.
Pain
- Mechanical pain – triggered by mobilising the joint.
- During activity, after long activity or at the end of the day.
- Can be stimulated by cold, trauma and fatigue.
Tenderness
- Usually palpated around the joint line
Limitation in joint movement
- You may be unable to move the joint through full range. This can be due to structural changes in the joint space due to disease progression.
Sounds
You may hear crackling, scraping, popping sounds. These may be due to the less smooth surfaces of the joint and changes in cartilage quality.
Mild Swelling
- Likely due to inflammation around the joint
Bony spurs
- Additional bits of bone can form around the affected joint.
(Mayo clinic, 2021; Arthritis Foundation 2023)
Diagnosis
Your history and signs and symptoms will give your physiotherapist a good idea if you have arthritis. For a definite diagnosis. your GP will be able to assess whether you have osteoarthritis. The GP can organise x-rays and might test blood to exclude other types of arthritis.
Treatment
The core treatments are therapeutic exercise and weight management, alongside information and support. (NICE guidelines, 2022)
Exercise:
- An exercise program tailored to your needs, and adhered to, will reduce pain, benefit the joints and improve function. Remember, motion is lotion for our joints!
- Did you know we run a group class to help with osteoarthritis symptoms in our studio? Let us know if you might like to join in this Happy Healthy Hearts and Bones program.
- Recent research (Burfield et a.l 2023) found that there is no increased prevalence/risk of developing knee OA in the running population in comparison to those that ran significantly less, so don’t be afraid to continue your running!
Weight management:
- If overweight, weight loss is likely to be beneficial in improving quality of life, reducing pain and improving physical function
Medication and surgery:
- Pharmacological therapies and surgery are available and can be discussed with your GP upon diagnosis.
- Surgeries are available and might be discussed with you if conservative management isn’t successful.
Information and support:
- It’s important to understand your condition and what you can do to self-manage as best you can.
- There are many resources out there that can help you learn about OA
- There are many support groups such as Arthritis Ireland that may be helpful.
Links to supports for you:
How can physiotherapy help?
We can help you manage your OA in many ways.
- Improve your knowledge and understanding of your condition and options.
- Creating a personalised and individualised exercise plan that can help:
- Improve muscle strength
- Reduce pain
- Improve range of motion
- Help improve muscle imbalances
- Assistive devices: If required, we can help with fitting and teaching how to use assistive devices effectively.
- Falls prevention strategies – Those with OA have an 30% increased risk of falls and 20% greater risk of fracture. By working on falls prevention exercises with your physiotherapist, this can reduce your risk of falling.
It’s important to note that your osteoarthritis may not be fully curable but, it most certainly can be managed very well. By discussing with your physiotherapist, we can help improve your quality of life and manage your symptoms.
Just because you have arthritis does not mean you have to have pain.
References:
Burfield, M., Sayers, M., and Buhmann, R. (2023) ‘The association between running volume and knee osteoarthritis prevalence: A systematic review and meta-analysis’,
Physical therapy in sport, 61, 1–10, available:
https://doi.org/10.1016/j.ptsp.2023.02.003.
Juan C Mora, Rene Przkora & Yenisel Cruz-Almeida (2019) ‘
Knee osteoarthritis: pathophysiology and current treatment modalities’, Journal of Pain Research, 11:, 2189-2196, DOI:
10.2147/JPR.S154002Page, C.J., Hinman, R.S., and Bennell, K.L. (2011) ‘
Physiotherapy management of knee osteoarthritis: Physiotherapy management of knee OA’, International journal of rheumatic diseases, 14(2), 145–151, available:
https://doi.org/10.1111/j.1756-185X.2011.01612.x.

 It has long been thought that cartilage once worn would not heal but now experts believe that that movement and walking can create more fluid flow around the joints and special cells called chondrocytes help cartilage repair and growth to occur (Moseley, Butler and Stanton, 2023). So instead of calling it ‘wear and tear’ let’s now call it ‘wear and repair’!
It has long been thought that cartilage once worn would not heal but now experts believe that that movement and walking can create more fluid flow around the joints and special cells called chondrocytes help cartilage repair and growth to occur (Moseley, Butler and Stanton, 2023). So instead of calling it ‘wear and tear’ let’s now call it ‘wear and repair’!